Health
Related: About this forumFungi Found in Brains of Alzheimer's Patients
Despite years of intense medical research, the cause of Alzheimer's remains enigmatic. The ultimate molecular manifestation of the disease consists of the accumulation of a small toxic protein called amyloid beta that causes inflammation and destroys neurons. Why this occurs in some individuals but not others is unknown. Genetic, immunological, and environmental risk factors have been investigated, but no smoking gun has emerged.
A relatively new hypothesis is that fungal infection can trigger the disease. Back in 2014, a group of Spanish researchers found fungal DNA and proteins in the brains of Alzheimer's patients. Now, the same team has performed a new analysis using fungus-specific antibodies. They show that several different fungi are present, both inside and outside cells, throughout the brains of Alzheimer's patients. (See figure.)
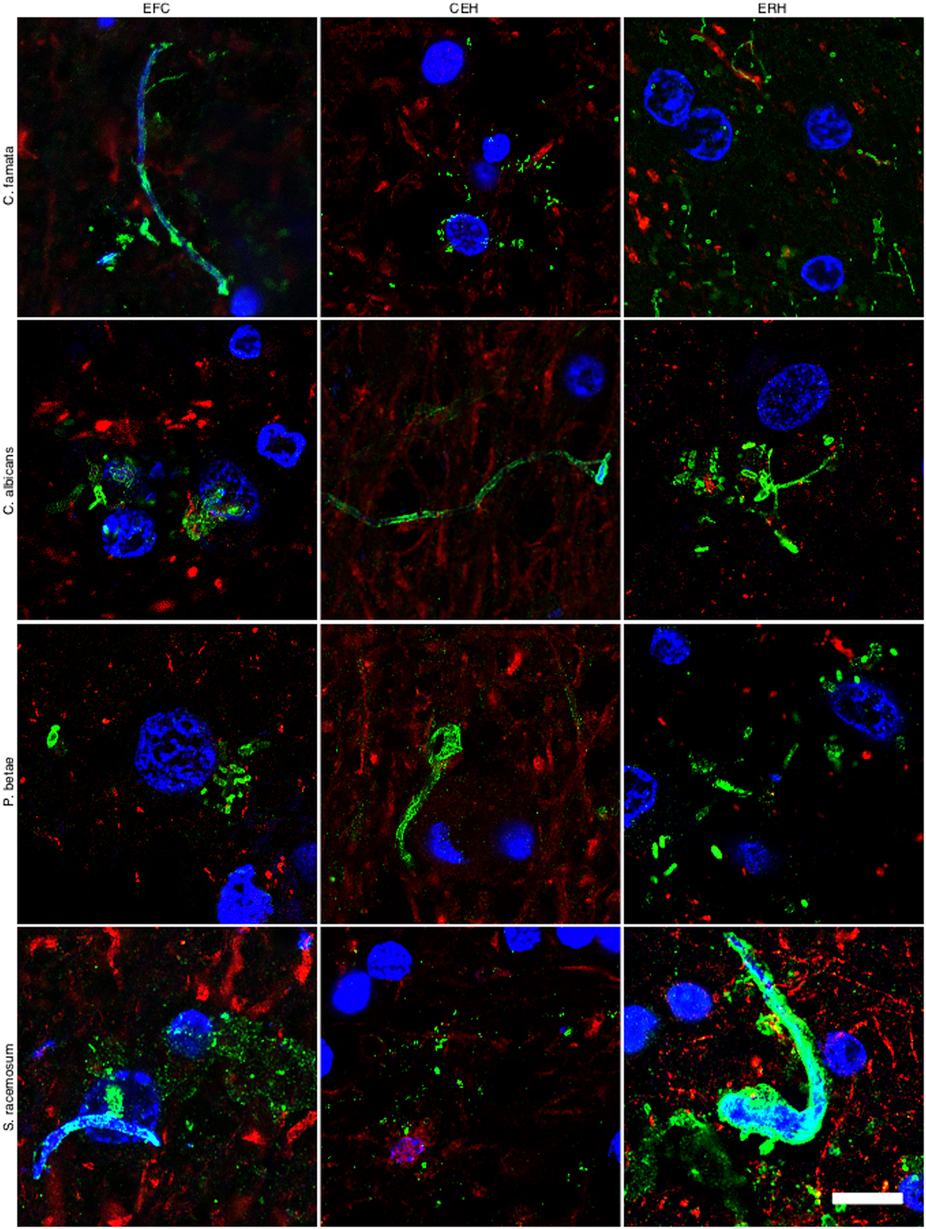
In the figure above, the authors stained (in green) various regions of an Alzheimer's brain with antibodies against four fungi: Candida famata, Candida albicans, Phoma betae, and Syncephalastrum racemosum. All samples were positive. The authors then performed PCR, a test that detects DNA, on ten additional brains with Alzheimer's. All contained fungi, while control (disease-free) brains did not.
So, does this constitute "slam dunk" evidence for a fungal cause of Alzheimer's disease? Unfortunately, no. There are still many questions that need to be answered. For instance:
1. Is fungal infection a cause or consequence of Alzheimer's? It is possible, if not likely, that people with Alzheimer's disease are so sick that their brains become susceptible to fungal infection. Under this scenario, fungus would be a consequence, not a cause, of Alzheimer's.
more
http://www.realclearscience.com/journal_club/2015/10/27/fungi_found_in_brains_of_alzheimers_patients_109425.html
d_r
(6,907 posts)concern #2, that there are many different types of fungi found, is support for #1, that a weakened brain may be more susceptible to fungal infection and so consequence not cause
PADemD
(4,482 posts)DreamGypsy
(2,252 posts)Fungal infections are estimated to occur in over a billion people each year, and recent evidence suggests the rate is increasing (Hsu 2011; Di Santo 2010; Brown 2012; Fungal Research Trust 2011). Fungi can infect almost any part of the body including skin, nails, respiratory tract, urogenital tract, alimentary tract, or can be systemic (Long 2009; Baron 1996). Anyone can acquire a fungal infection, but the elderly, critically ill, and individuals with weakened immunity, due to diseases such as HIV/AIDS or use of immunosuppressive medications, have a higher risk (Hsu 2011; Baddley 2011).
Although several species of fungi are potentially pathogenic in humans, candida (esp. Candida albicans) is the organism responsible for most fungal infections. Candida, which is normally present within the human body, is usually harmless. However, it can cause symptoms when a weakened immune system or other factors allow it to grow unabated (Merck Manual 2008; Cheng 2012; Douglas 2011).
Increased use of antibiotics and immunosuppressive drugs such as corticosteroids are major factors contributing to higher frequency of fungal infections. Antibiotics and immunosuppressive drugs, by disrupting normal bacterial colonization and suppressing the immune system, create an environment within the body in which fungi can thrive (Hsu 2011; Tani 2012).
Fungal infections can range in severity from superficial to life-threatening. For example, fungal infections affecting only the top layers of the skin are readily treatable and have a relatively limited impact on quality of life. However, if a fungal infection enters systemic circulation, consequences can be deadly (Badiee 2011; Zuber 2001).
...more at the link.
question everything
(47,462 posts)This is why it is so difficult to prescribe medications that would enter the brain.
Unless the membrane of the brain of Alzheimer's patients is leaky - I think that it was speculated once - and thus allows foreign biologics to enter.
DreamGypsy
(2,252 posts)...
First, specifically relating to yeast, from 2001: Traversal of Candida albicans across Human Blood-Brain Barrier In Vitro:
Abstract
Candida albicans is an opportunistic pathogen, which primarily affects neonates and immunocompromised individuals. The pathogen can invade the central nervous system, resulting in meningitis. At present, the pathogenesis of C. albicans meningitis is unclear. We used an in vitro model of the human blood-brain barrier to investigate the interaction(s) of C. albicans with human brain microvascular endothelial cells (BMEC). Binding of C. albicans to human BMEC was time and inoculum dependent. Invasion of C. albicans into human BMEC was demonstrated by using an enzyme-linked immunosorbent assay based on fluorescent staining of C. albicans with calcoflour. In contrast, avirulent Candida mutant strains and nonpathogenic yeast Saccharomyces cerevisiae were not able to bind and invade human BMEC. Morphological studies revealed that on association with human BMEC, C. albicans formed germ tubes and was able to bud intracellularly. Transmission electron microscopy showed various stages of C. albicans interactions with human BMEC, e.g., pseudopod-like structures on human BMEC membrane and intracellular vacuole-like structures retaining C. albicans. Of interest, C. albicans was able to bud and develop pseudohyphae inside human BMEC without apparent morphological changes of the host cells. In addition, C. albicans penetrates through human BMEC monolayers without a detectable change in transendothelial electrical resistance and inulin permeability. This is the first demonstration that C. albicans is able to adhere, invade, and transcytose across human BMEC without affecting monolayer integrity. A complete understanding of the interaction(s) of C. albicans with human BMEC should contribute to the understanding of the pathogenic mechanism(s) of C. albicans meningitis.
<big snip>
DISCUSSION
Meningitis occurs in humans infected with C. albicans, indicating that this microorganism is able to breach the BBB (12, 46). Despite intensive studies on the pathogenicity of C albicans, the mechanism by which this organism invades the CNS and causes meningitis is little understood. Since the brain microvascular endothelium is the major site of the BBB, C. albicans must be able to cross human BMEC to cause CNS infection. There are several possible ways by which C. albicans could penetrate the endothelial barrier: (i) via a paracellular route by crossing between the adjacent endothelial cells, (ii) via direct invasion of the endothelial cells and subsequent release from the basolateral side, (iii) indirectly via migration of the yeast infected monocytes across the endothelial barrier, or (iv) via destruction of the endothelial barrier by affecting the integrity of the BBB endothelium. To our knowledge, no information is available concerning which mechanism(s) is operative in the traversal of C. albicans across the BBB. In the present study, our investigation of the interaction of Candida cells with human BMEC showed for the first time that C. albicans adheres to, invades, and transcytose across human BMEC monolayers without altering their integrity.
In vitro systems to study the invasion of human BMEC by bacterial pathogens, using a gentamicin protection assay, have been previously described by our group (3, 22, 32, 39). Unfortunately, a similar antimicrobial protection assay cannot be applied to yeast systems because no specific and effective antifungal drugs to kill extracellular yeasts are available (42, 43). To distinguish between adhesion to and invasion of human BMEC by C. albicans, we developed an ELISA-based fluorescence assay to determine relative invasion and total cell-associated yeast by using the properties of the dye CWF (5). CWF is a small fluorescent dye, which can specifically stain yeast cell wall components, e.g. chitin and glucans, which are absent from mammalian host cells. In addition, CWF does not penetrate live mammalian cells but is able to enter fixed and permeabilized host cells effectively and consequently stain intracellular yeast. We showed that CWF could be used effectively to stain yeast without appearing to stain the human BMEC. The relative contributions of adhesion and invasion can therefore be determined from the differences in the fluorescence reading between permeabilized (total cell-associated yeast) and nonpermeabilized (extracellular yeast) host cells. Our data indicate that Candida can adhere to and invade human BMEC very robustly. We consistently observed that approximately 30 to 50% of the total cell-associated C. albicans represents invaded organisms. In contrast, no such binding and invasion was observed for S. cerevisiae.
The initial step in establishing contact with host cells is the adherence of Candida to the host cell membrane, which is likely to play a critical role in withstanding blood flow in vivo. Our morphological studies showed that C. albicans often attached to the apical surface of human BMEC in clusters with long germ tubes protruding upward. This so-called arborization of C. albicans colonies seems a unique feature of this organism. Invasion of human BMEC by Candida had no noticeable effect on cells and monolayer integrity, since BMEC morphology, ApopTag staining, inulin permeability, and TEER gave results similar to those for the uninfected control cells. In addition, trypan blue was excluded by monolayers incubated with C. albicans. In contrast, penetration of C. albicans into HUVEC was found to induce cellular injury of the HUVEC (14, 16) but caused no visible changes in the architecture of the HUVEC microtubules. Studies are in progress to examine these apparent differences between human BMEC and HUVEC in response to C. albicans.
The morphological characteristics of C. albicans invading human BMEC were further studied by TEM. Invasion of human BMEC by C. albicans involved protruding contacts and membrane engulfment, similar to the zipper mechanism of the host cell surface around C. albicans trapped in intracellular vacuoles (19). Other possible mechanisms of pathogenic invasion, e.g., membrane ruffling (4, 15), pedestal formation, or coated-pit formation (37), were not observed in the invasion of human BMEC by C. albicans in these studies, although we could not rule out the possibility that they could be involved under different physiological or pathogenic conditions. Intracellular survival is a challenge for most pathogens, yet C. albicans seems to adapt well in human BMEC. TEM studies showed that the intracellular C. albicans organisms were located within a vacuole-like structure and were able to bud and develop psuedohyphae within vacuoles. These findings differ from those for meningitis-causing bacteria, such as E. coli and group B streptococci, where there is no evidence of intracellular multiplication within human BMEC. In contrast, we showed that Citrobacter was able to replicate within human BMEC vacuoles (3). Compared to bacterial pathogens, Candida may have some advantage(s) in surviving in host cells by being able to bud or form pseudohyphae intracellularly in vacuoles. The optimal pH for yeast growth is around 5, which is close to the pH in endosomal vacuoles, and this may contribute to the survival and budding of C. albicans within human BMEC.
From our binding and invasion assays and our TEM and transcytosis data, it became clear that C. albicans was able to invade human BMEC from the apical side, cross the BMEC, and exit from the basolateral side. The nature of the trafficking mechanisms(s) is unclear, but the exit of C. albicans cells from the basolateral side could occur by exocytosis of budded yeast or by growth of germ tubes across the human BMEC monolayer. Although we occasionally observed some internal Candida cells associated with disrupted human BMEC membrane, we could not conclude that the disrupted membrane was due to (i) sample preparation or (ii) lysis by Candida cells. Further study is required to clarify this observation. Interestingly, transcytosis of C. albicans occurred with no effect on the integrity of the human BMEC monolayer. In accordance with our observation, a previous study using bovine aortic endothelial cells (AEC) (48) showed that C. albicans cells were in yeast form in the initial phases of association with bovine AEC. Fungal cells were rarely observed between endothelial cells, and evading cells were shown to form hyphal extensions. However, the bovine AEC monolayer gradually loses its integrity during C. albicans transmigration (48). Together, these results suggest that the primary route of Candida traversal across the endothelial cells is a transcellular pathway but the effect of the Candida transcytosis on the endothelial cell integrity may differ between human BMEC and bovine AEC.
At present, it is unclear what structures of C. albicans contribute to binding, invasion, intracellular replication, and transcytosis in human BMEC. Multiple fungal factors have been implicated in the pathogenesis of C. albicans infections. These include genes for adherence capacity (ALS1-9, HWP1, INT1, etc.) (17, 18, 20, 21, 38), phenotypic switching (EFG1, CPH1, TUP1, etc.) (6, 28), transition between blastospores and hyphal forms (CEK1, COS1/NIK1, HK1, SSK1, HOG1, RSR1, CLN1, CST20, HST7, CLA4, etc.) (1, 2, 8, 9, 11, 25, 26, 29, 44, 45), hydrolytic enzymes (PLB1) (27, 34) and secreted aspartyl proteinases, SAP1-SAP9 (23, 31, 36). We have so far tested two mutants, hOG301 and CHK21 (?cahk1). Our preliminary findings indicate that these mutants have lost their ability to adhere to or associate with human BMEC (Fig. Fig.1A).1A). It is not known whether the defect(s) is due to their primary function (loss of invasive ability) or to a secondary effect (morphological aberration, etc.). Additional studies are needed to find which structures of C. albicans contribute to their interactions with human BMEC. In summary, we showed that C. albicans adheres to and invades human BMEC and is able to bud or form pseudohyphae inside human BMEC and traverse the BMEC without affecting the integrity of the monolayer. The mechanism of crossing human BMEC monolayer is likely to involve a transcellular pathway.
And from earlier this year, in a report from the Cure Alzheimer Fund New Insights Into the Blood-Brain Barrier:
Three recent discoveries by University of Southern California neuroscientist Berislav Zlokovic, M.D., Ph.D., have clarified one of the least-understood elements of Alzheimer’s disease: how the blood-brain barrier becomes compromised and contributes to the disease process.
<snip>
The discoveries by Zlokovic—director of the Zilkha Neurogenetic Institute and professor and chair of the Department of Physiology and Biophysics at the University of Southern California, Keck School of Medicine, Los Angeles, and a member of the Cure Alzheimer’s Fund Research Consortium since 2011—bring us one step closer:In January, Zlokovic’s team was able to use high-resolution imaging of the living brain to show, irrefutably, that the BBB becomes leaky with age, starting in the area of the hippocampus—the area responsible for memory and learning that is affected very early in Alzheimer’s disease. This leakiness begins long before there are any cognitive symptoms. The discovery, published in the journal Neuron, suggests that specialized brain scans might, in the near future, help doctors routinely spot very early, presymptomatic warning signs of dementia. It also identified early injury to brain vascular cells called pericytes, a type of mural cell that surrounds brain capillaries and acts as a “gatekeeper” of the blood-brain barrier.
In March, Zlokovic’s team discovered that deficiency of a key BBB protein called GLUT1, which helps move glucose, a major energy substrate for the healthy brain, across the BBB, is directly connected to a compromised barrier. It also suggested that the gene regulating this protein could be an excellent drug target. The discovery was published in the journal Nature Neuroscience.
In May, Zlokovic discovered the mechanism of action for an Alzheimer’s-implicated gene encoding protein known as PICALM. The PICALM-Alzheimer’s connection had been studied previously by Cure Alzheimer’s Research Consortium Chair Rudy Tanzi, Ph.D., and Zlokovic in a Cure Alzheimer’s Fund-supported study. Zlokovic, publishing his research in Nature Neuroscience, showed that PICALM is crucial for clearing Abeta across the BBB. PICALM variants associated with increased risk for Alzheimer’s lead to diminished expression of PICALM and faulty clearance of Abeta from the brain, leading to its accumulation both in the human brain and animal models of the disease. This suggests that, while Abeta is crucial in the subsequent cascade that leads to Alzheimer’s disease, the compromise of the BBB may happen earlier in the process, and may contribute directly to the destructive excess of Abeta in the brain.
“The brain cannot function in the presence of blood-brain barrier breakdown,” said Zlokovic. “Now we know that not only is Abeta important in Alzheimer’s, but also that this barrier, which is regulating transfer of molecules between the brain and blood, and vice versa blood and brain, can become leaky and dysfunctional and lead to subsequent problems likely contributing to onset and progression of dementia.”
Jeffrey Morby, chairman of Cure Alzheimer’s Fund, added, “We created our Research Consortium in order to spur innovation through the speedy sharing of vital data between top researchers. Dr. Zlokovic’s latest advance with PICALM is a perfect example of what we’ve been able to do, and it brings us that much closer to a cure.”
...
Hope this helps, DG
KT2000
(20,572 posts)the blood-brain barrier. There are instances where it can be breached such as under stress. Certain chemicals and pharmaceuticals are also capable of that sometimes allowing other substances to hitch a ride. Possibly decades of small breaches can build up until there is a tipping point.
Also something to consider is the olfactory bulb which sits deep in the brain. In the nose. the cells have tight junctions that prevent passage of toxic substances. In people exposed to certain chemicals such as sulfuric acid, the tight junctions are compromised - loose.
question everything
(47,462 posts)TwilightGardener
(46,416 posts)I wonder if the fungi lodge in the brain because the structure of the brain and brain cells, plus the amyloid tangles, trap the fungus that might be in the bloodstream--some kind of low-grade septic fungal infection that lodges in the brain and doesn't cause an immune response? Or maybe the altered brain structure and chemistry of Alzheimers are a result of low-grade inflammation from fungi? Really interesting, lots of directions you could take off in with this.